Abstract
Introduction:
Recently, we showed that in chronic myeloproliferative neoplasia (CMN), β1 and β2 integrins are overactivated on leukocytes in patients and in a JAK2-V617F knock-in mouse model (Gupta et al., Leukemia, 2017; Edelmann-Stephan et al., JCI, In-Press Preview) resulting in increased adhesion of leukocytes to vascular cell adhesion molecule 1 (VCAM-1) and to intercellular cell adhesion molecule 1 (ICAM-1). VCAM-1 and ICAM-1 are abundantly expressed on endothelial cells and in spleen tissue. In JAK2-V617F induced CMN, current therapeutic strategies for symptomatic splenomegaly as hydroxyurea, JAK inhibitors or allogeneic stem cell transplantation (SCT) are effective, however, often limited in duration of efficacy or in eligibility for SCT. Therefore, there is a need to deeper understand the pathophysiology of splenomegaly in CMN in order to develop novel therapeutic approaches. We sought to investigate the effects of in vivo blockade of β1 and β2 integrin overactivation on spleen size, cellular composition of spleen and peripheral blood counts.
Material and Methods:
11 weeks old Vav1-Cre x JAK2+/V617F mice were treated with a combination of 200µg neutralizing anti-α4β1-integrin (VLA4) antibody (BioXCell, USA) plus 200µg neutralizing anti-β2 integrin antibody (BD Pharmingen, USA) (N=6) and with isotype controls (each 200µg) (N=3), respectively. Animals were injected i.p. on day 1 and day 8. Small animal MRI was used to serially assess the development of spleen volume on days 1, 8, and 15. Abdominal MRI-images employing a slice thickness of 1-2 mm were obtained. The volume of spleens were computed according to radiology standards. Peripheral blood was collected via retro-orbital bleeding and blood counts were measured on days 1, 8, and 15. Thereafter, mice were sacrificed by cervical dislocation and spleens were removed for further analysis by FACS.
Results and Discussion:
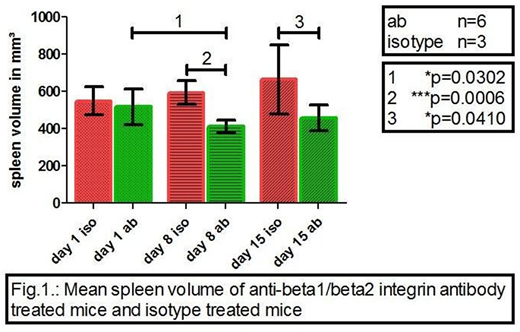
The applied antibody injections were well tolerated and all animals survived the planned observation period. At the start of the experiments (day 1), splenomegaly was confirmed by MRI. As expected, the spleen volumes were similar in the cohorts of isotype and β1/β2 integrin antibody treated JAK2+/V617F mice: 550±76 mm3 (mean±SD) and 518±96 mm3, respectively (Fig. 1). At day 8, upon a single injection of β1/β2 integrin antibodies, a significant decrease in mean spleen volume from baseline 518±96 mm3 to 414±32 mm3 (p=0.0302) was observed (Fig. 1). The correspondent mean±SD for the isotype antibody treated animals was 594±63 mm3. Thus, on day 8, a 30.3% reduction in spleen volume was demonstrated upon β1/β2 integrin antibody treatment in comparison to isotype treatment (p=0.0006). On day 15, the mean spleen volumes of isotype-treated and β1/β2 integrin antibody-treated mice were 665±187 mm3 and 460±69 mm3 (p=0.0410). These results demonstrate that in JAK2-V617F induced disease, blocking of overactivated β1/β2 integrins reduces splenomegaly within a short period of time (8 days). Longer application schedules may build up even stronger and stable decrease in spleen size.
In addition to MRI imaging, we also analyzed the composition of peripheral blood cells. At the start of the experiments on day 1, blood parameters showed the typical abnormalities of myeloproliferative disease in both cohorts. Mean counts in isotype treated animals were: WBC = 14,300/µL, hematocrit = 80.3 %, PLT = 1283/nL. Mean counts in β1/β2 integrin antibody treated animals were: WBC = 13,850/µL, hematocrit = 76.0 %, PLT = 1348/nL. This confirms that the JAK2-V617F mouse model used indeed resembles polycythemia vera. In general, the changes observed upon β1/β2 integrin antibody treatment in blood were subtle: the WBC slightly decreased from 13,850/µL to 12,520/µL on day 15, whereas RBC, HCT and PLT remained nearly unchanged. This indicates tolerability of β1/β2 integrin antibody treatment at the level of the hematopoietic system. In isotype treated mice, peripheral blood counts also stayed stable. Data obtained by FACS analysis of peripheral blood and of spleen tissue (composition in granulocytes, B-cells and T-cells) will be presented.
Overall, our results indicate a novel role of JAK2-V617F induced overactivation of β1/β2 integrins in development of splenomegaly. Thus, modulation of integrin activity may have therapeutic potential to reduce the spleen volume in CMN patients insufficiently responding to standard treatment.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal